TREATMENT
Please find the procedures on carrying out urgent dental treatment in COVID-19 pandemic
When all options have been exhausted via remote management and the only way to appropriately manage the patient is by face to face treatment, patients are subsequently refered to the most appropriate treatment clinic according to the patient type, their needs and capacity of service centres using current pathways in place.
All face to face management should be in adherence with standard operating procedures local and national including NHS standard operating procedures for COVID-19
KEY ASPECTS:
Prior to commencing face to face treatments a risk assessment must be undertaken [NIGHT DENTAL RISK ASSESSMENT TEMPLATE]
Patient Flow
Patient flow should be smooth, one way where possible with minimal touching of surfaces and separate entry and exit where possible.
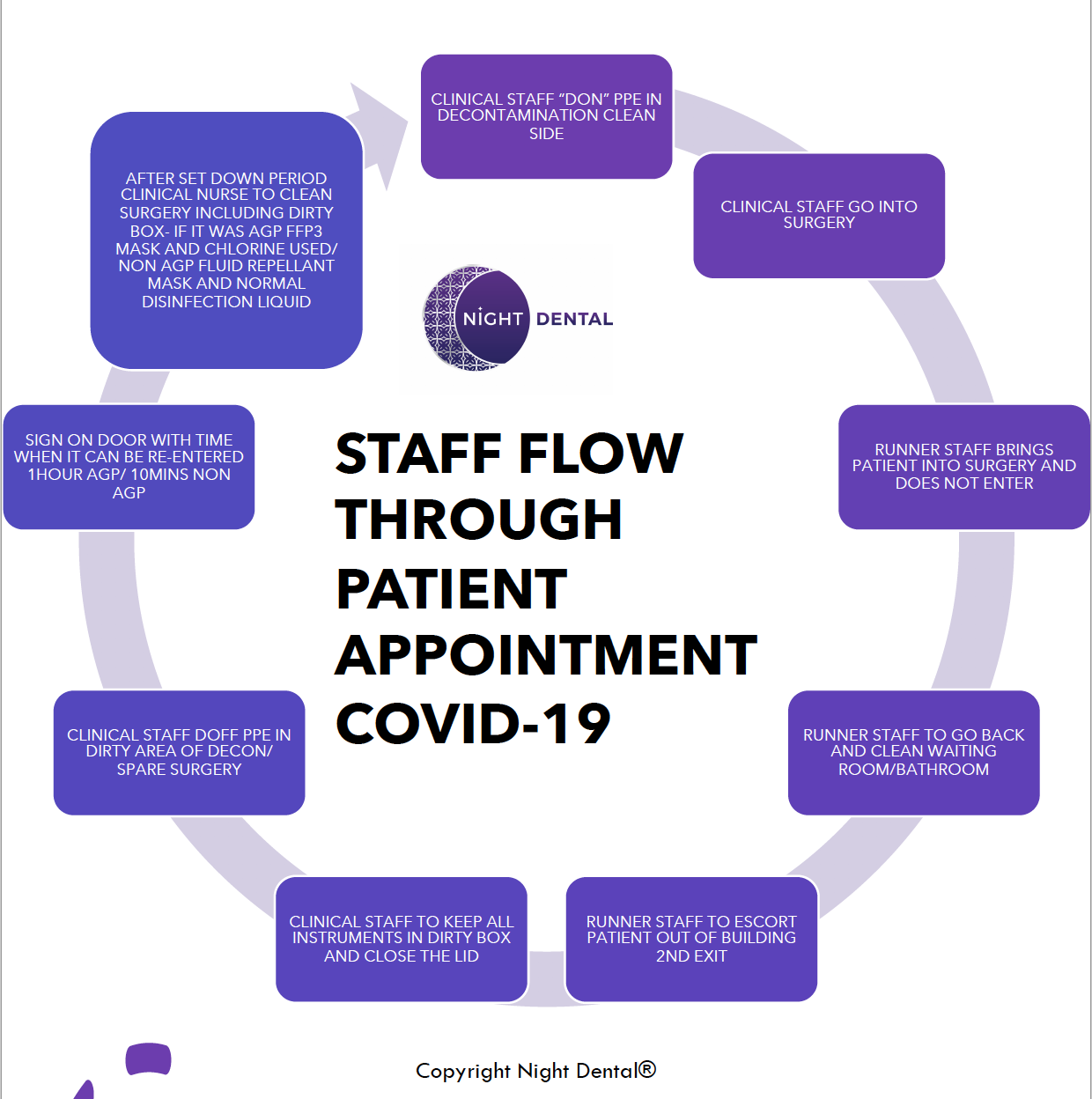
There should be allocated donning and doffing stations for PPE
The patient flow is is set and rehearsed with test runs. Adapted according to findings in test runs. There should be appropriate "zoning" through the clinic separation for "donning" and "doffing" as well as temporal and spatial separation for different groups of patients [e.g vulnerable patients booked first appointments with no other patients in clinic]
Workflow should be practiced and rehearsed several times and improved upon if any concerns are found
Maps drawn up to show this flow and zoning for each site. Please see flow through map [NIGHT DENTAL SITE XXX FLOW MAP]
Protocols
CLICK BELOW
- Prior to patient arrival at booking stage patient should be asked regarding COVID-19 Status & asked to update immediately on a change in status [SEE COVID-19 STATUS CHECKER]
- Patient complaint recorded any change in need/concern is recorded
- Medical History checked
- Exempt status checked
- Payment for treatment taken over the phone where applicable. Where this is not possible patient advised to put exact change in a clear wipeable bag on arrival, patient advised they will not be seen without full pre-payment
- Full patient service instructions given orally and where possible written copy emailed to patient [SEE PATIENT INSTRUCTIONS]
- Patient should be reminded not be bring an escort unless necessary such as a parent with a child in which case only one escort brought from patient's household where possible
- Patients advised not to bring any belongings bags & coat inside
- Online/ phone translator service should be arranged [TRANSLATORY SERVICE]
- Risk assess according to the individual patient needs and best interest
- Information should be gathered to allow comprehensive pre-treatment planning on what treatment may be required including whether it would be AGE/NON-AGE
- A digital pack should be prepared and sent to patients where applicable to include:
(patient questionnaire, medical history, FP17, risk assessments, patient preparation information, consent forms and payment methods for patients/carers to complete and return in advance of their visit)
- Patient asked to wait in the car or outside 2metres from any other person & contact clinic via phone or knock to register their arrival
- Maintaining 2metre social distancing throughout the whole patient flow except for treatment and assessment and kept as minimal and short as possible
- Patient called to ask to enter the building and to wash hands on arrival any escort is also to wash their hands
- Temperature of patient taken using non contact thermometer [NB: This may be unreliable]
- If pre-payment not taken patient cash collection in a wipeable bag
- Patient given instructions on patient flow
- Patient who have bought belongings are advised to leave belongings out of the clinic such as in a car or with an escort otherwise offer to store where feasible however explain there is no responsibility with the clinic for items lost or stolen
- Where digital versions have not been obtained Medical History and PR1/ FP17 forms checked filled and signed by staff and signed as [COVID-19]
- Where a parent or guardian could not attend due to vulnerable/shielding they should be contacted via phone to confirm consent
- Parents and guardian/ escort at this point advised to wait back outside where possible
- Appropriate chaperoning must be considered
- Patient is led into surgery by runner staff/ "clean" nurse
Patient must be refused service if
- Displaying COVID-19 symptoms
- No longer has an urgent need
- Failure to provide pre-payment
- Failure to follow instructions given
- Full donning is carried out for the clinical staff
- Surgery kept bare
- All items that are required for the anticipated treatment are all laid out in the clean area of the surgery with wipeable cover/ in sterilised pouches
- Items that may be required are accessible via Runner staff/ "clean" nurse who will pass items via trolley
- A trolley is kept outside the surgery
- When an item is needed a runner nurse is notified via a knock/ walkie talkie or intercom and will place on top of the trolley and the "dirty" assisting nurse will collect from the trolley
- The runner nurse must never enter the surgery at any point
- Treatment is kept as minimal and short as possible to address urgent need and prevent repeat visits for the same need where possible
Suggested Protocol for Developing Radiographs
For wet film and phosphor plate radiographic films:
1 "Dirty" nurse places cleaned radiographic film in a sealed box sitting on the trolley or held by ‘clean’ nurse outside surgery
2. "Clean’ nurse" disinfects it, removes barrier protection and develops radiograph/ where self developing radiographs are used these are processed within the surgery by "dirty" nurse
HIGH RISK AEROSOL GENERATING PROCEDURES
Are procedures that are at high risk of causing aerosol generation. High speed drills water from triple air syringes 3-in-1 syringes, Ultrasonic scalers, Surgical extractions access of cavity such as for extirpation
They should treatment should be avoided and delayed to when national COVID-19 alert level is reduced were possible
- Runner nurse opens surgery door from outside to allow patient entry
- Surgery space is kept bare
- Escort should not enter the treatment room
- PPE should be worn and donned according PHE guidance, please see PPE page
- All extra items that may be needed kept on a trolley outside the surgery
- No paper notes or other paper left out
- Digital clinical records may be completed in the surgery while wearing PPE, or in a clean area following doffing of PPE and hand hygiene. If not washable, the keyboard and mouse should be covered with single-use cling film.
- Surgery door kept shut throughout procedure and if there is a window, it is kept open
- Runner / "clean" nurse passes items to operating staff when required
- A rubber dam should be placed over the tooth and sealed well
- High power suction aspirator [where available] should be used as far as possible this can reduce aerosol produced
- Decontamination of the whole operative field, to include rubber dam and tooth, with sodium hypochlorite
- Robust infection control should be adhered throughout procedures in line with Standard infection control procedures and COVID-19 transmission based infection control procedures
- Patient asked to leave and where ever possible asked to leave out a separate exit from surgery and to sanitise /wash hands on exit
- Treatment should be completed in one visit where possible
- Respirators and final close eye protection should not be touched or removed in the room at any point during the procedure or after the procedures
- Doffing of PPE at appropriate station
- Room vacated for 1hr following end of aerosol exposure if the room is needed sooner please follow latest PHE guideline
- Terminal clean as outlined infection control page should include mopping of the floor
- Post treatment the instrument box should be covered and left in the surgery
- Clinicians should go to doffing station & follow doffing guidelines, they must leave the clinical room with their eye protection and respirators still on.
- After a full hour has been given a terminal clean of full surgery doors, door handles any surfaces that are at risk of contact including floor using appropriate cleaning agent effective against enveloped viruses such as 1000ppm chlorine mix OR alternative disinfection effective against enveloped virus by "dirty nurse" with a FFP3 respirator on
- Post treatment disinfection should follow HTM: 01-05
Suggested Protocol if a Patient becomes unwell during an appointment in a UDC
If COVID-19 is considered possible when an appointment is already in progress, assess a suitable and safe point to bring any treatment to a close.
1. Isolate patient in surgery you are treating away from other patients. Provide mask and gloves for the patient and chaperone to put on. Provide water and tissues. Advise others not to enter the area. Put out isolation notices to prevent entry
2. If the patient is critically ill or requires emergency medical care, an ambulance should be requested, and the 999-call handler informed of COVID-19 risk. Normal medical emergency training is appropriate especially oxygen and asthma care if appropriate. Support breathing as primary concern.
3. Otherwise withdraw from the area, wash hands thoroughly with soap and water. Change PPE and discard in clinical waste. Don new PPE and apron.
4. If they are so unwell they cannot leave ask them where they have been in the building and clean all touched surfaces, open all doors, and windows. Turn up heating. Recruit help for other duties, such as reception.
5. Send all other patients home after updating their contact numbers/details. Once patients gone, shut practice. Put up PRACTICE CLOSED sign on front door.
6. Advise patient to contact NHS111 from their mobile in designated isolation area: –patient will need to state where they are calling from and provide contact details for the practice. If no patient mobile, staff to call on practice phone and relay responses to NHS111.
7. While waiting for advice from NHS111, communicate with the patient from outside area to check status. If you need to enter the area, wear personal protective equipment (PPE) in line with standard infection control precautions, gloves, disposable apron and surgical mask and keep exposure to a minimum. All PPE should be disposed of as clinical waste.
8. If a healthcare professional is required to enter the area to offer assistance, they should wear disposable gloves, disposable aprons and fluid-resistant surgical facemasks.
9. When patient has left the building, clean surgeries thoroughly and ALL communal areas down to front door and time allowed for aerosols to settle.
INFECTION CONTROL:
Standard infection control- Standard Infection Control Procedures (SICPs) are infection control precautions that are applicable at all times in a dental care setting according to guidance from HTM 01-05, CQC, NICE, SDCEP.
Transmission based cross infection protocols- In addition to SICPs, transmission based precautions (TBPs) are application specific to the current pandemic and prevention of transmission according to the route of transmission
Transmission Based Procedures look at the additional cross infection procedures introduced as a direct result of and to protect against COVID-19.
These look directly at the transmission behaviour of the virus and are steps adopted to prevent and minimise the risks of these transmissions.
SUMMARY OF COVID-19 PREPARATIONS
Please see a summary list of extra measures we have in place for how these are implemented refer to treatment page.
The introduction of adjuncts should be risk assessed and considered and this will vary clinic to clinic however here is a list of additional measures that may be considered please follow latest guidelines where these change. Not all have evidence to back their use so use at your own discretion please order your COVID-19 supplies, PPE supplies and floor signs via www.themedstock.com :
- Posters reminding patient of instructions e.g washing hands/ social distancing/ staying at home if displaying COVID-19
- Patient instruction sheets/videos
- Hydrogen peroxide 1% /iodine mouthwashes no longer advised
- Using rubber dams for all teeth that are opened
- Trolleys
- Screens for reception
- Touch free thermometers [NB: Can be unreliable on its own as risk assessment in determining patient status]
- One way system and signage with separate entrance and exit where possible
- Walkie-talkies or intercoms from surgery to runner staff communication
- Wipeable door label
- Floor signs to mark where patient should be waiting
- 1000ppm Chlorine based disinfection or alternate disinfection effective against enveloped viruses
- Mechanical ventilation extracting at a rate of 6 air changes an hour or above
- Donning and doffing stations with posters and instructions
- Videos showing patient flow/ donning & doffing
- Maps with patient walkthrough
- Resus UK posters for COVID-19 Protocols
- Treatment must be efficient
- PPE according to latest guidelines
- Keeping area ventilated close surgery door and open windows
- Do not use A/C do not use fans that recirculate the air
- Digital clinical records may be completed in the surgery while wearing PPE, or in a clean area following doffing of PPE and hand hygiene. If not washable, the keyboard and mouse should be covered with single-use cling film.
- EYE PROTECTION AND RESPIRATORS SHOULD ONLY BE REMOVED OUTSIDE SURGERY
- One hour "fallow time" following cessation of high risk AGEs
- Only use approved reusable gowns
- Where reusable gowns are used please use washer/dryers on site
- Surgery decontaminated after every patient interaction
- Toilets use out of use except for hand washing and patients with disability requirements and must be cleaned regularly (patient advised before hand)
- Wiping down door handles
- Reception and waiting rooms out of use where possible
- Shielding/vulnerable patients first thing & advised to wear a mask
- The type of treatment needs to considered and appropriate PPE planned
- Emergency stations are outside clinical rooms please make yourself familiar with drugs and dosages
- Reusable masks with appropriate filters are available, however, it is important that doffing and disinfection of these masks is carried out following a strict protocol to prevent contamination.
- [ Use of antibody/antigen screening may be considered in the future as aspiration ]
PATIENT SAFETY
Suggested Protocol if a Patient becomes unwell during an appointment in a UDC
If COVID-19 is considered possible when an appointment is already in progress, assess a suitable and safe point to bring any treatment to a close.
1. Isolate patient in surgery you are treating away from other patients. Provide mask and gloves for the patient and chaperone to put on. Provide bottle of water and tissues. Advise others not to enter the area. Put out isolation notices to prevent entry
2. If the patient is critically ill or requires emergency medical care, an ambulance should be requested, and the 999-call handler informed of COVID-19 risk. Normal medical emergency training is appropriate especially oxygen and asthma care if appropriate. Support breathing as primary concern.
3. Otherwise withdraw from the area, wash hands thoroughly with soap and water. Change PPE and discard in clinical waste. Don new PPE and apron.
4. If they are so unwell they cannot leave ask them where they have been in the building and clean all touched surfaces, open all doors, and windows. Turn up heating. Recruit help for other duties, such as reception.
5. Send all other patients home after updating their contact numbers/details. Once patients gone, shut practice. Put up PRACTICE CLOSED sign on front door.
6. Advise patient to contact NHS111 from their mobile in designated isolation area: –patient will need to state where they are calling from and provide contact details for the practice. If no patient mobile, staff to call on practice phone and relay responses to NHS111.
7. While waiting for advice from NHS111, communicate with the patient from outside area to check status. If you need to enter the area, wear personal protective equipment (PPE) in line with standard infection control precautions, gloves, disposable apron and surgical mask and keep exposure to a minimum. All PPE should be disposed of as clinical waste.
8. If a healthcare professional is required to enter the area to offer assistance, they should wear disposable gloves, disposable aprons and fluid-resistant surgical facemasks.
9. When patient has left the building, clean surgeries thoroughly and ALL communal areas down to front door and time allowed for aerosols to settle.
Safeguarding
Members of the urgent dental care team are in a position where they may identify the signs of abuse or neglect or hear something that causes them concern.
The following sites may be useful
Safeguarding resources for primary care
https://www.gov.uk/report-domestic-abuse
https://www.gov.uk/government/publications/safeguarding-in-general-dental-practice
Free NHS Safeguarding App http://www.myguideapps.com/projects/safeguarding/default/ which has local safeguarding contacts
COVID-19 and safeguarding overview https://elearning.rcgp.org.uk/pluginfile.php/149180/mod_resource/content/2/COVID-19%20and%20Safeguarding%20%286%29.pdf
E-learning
Child/adult course links to level 4
https://elearning.rcgp.org.uk/mod/page/view.php?id=8755https://portal.e-lfh.org.uk/Catalogue/Index
https://portal.e-lfh.org.uk/Catalogue/Index
• Safeguarding guidelines
https://elearning.rcgp.org.uk/mod/page/view.php?id=9382
• Support for domestic abuse victims
There is now a freephone, 24 hour National Domestic Abuse Helpline number – 0808 2000 247 – run by @RefugeCharity #YouAreNotAlone
Campaign assets can be accessed here https://www.dropbox.com/sh/2ldeo76tr71n7uv/AACN1t1dDsXb1wb2coyQvLIOa?dl=0
https://www.nationaldahelpline.org.uk/