Risk Assessing during COVID-19
Please note this is a summary guidance to our staff and must be used alongside full guidance linked. Find the guidance on carrying out general dental treatment in COVID-19 pandemic by FGDP uk and follow updates
The FGDPuk stress the use of a risk assessement based model with evidence backed framework
KEY ASPECTS:
RISK MATRIX SUMMARY
CLICK BELOW
- Up to date information should be available on line and widely disseminated to patients
- Patient communication ahead of dental practice visit is vital
- Digital communication should be encouraged but other methods made readily available
- Administrative tasks should be undertaken ahead of the visit where possible and should include:
- Patient questionnaire
o COVID Screening
o Medical history
o Patient forms – FP17, estimate, consent
o Information on payment - Review of technology should be considered with appropriate support and training put in place
- A digital pack should be prepared and sent to patients where applicable to include:
- (patient questionnaire, medical history, FP17, risk assessments, patient preparation information, consent forms and payment methods for patients/carers to complete and return in advance of their visit)
- Communicate arrangements & protocol for social distancing
- Minimise contamination of public areas by
- Offering storage of bags, coats, etc
- Provide antiseptic hand gel on entrance and exit
- Minimise waiting times in common areas
- Discourage use of toilet facilities
- Adoption of high level of infection control and prevention
- Protection of reception staff by social distancing, wearing of appropriate PPE and / or barrier screens
- Appointment times tailored to new ways of working
- Temporal and spatial zoning for vulnerable patients
- Temperature checks deemed unreliable
- Testing seen as aspirational
- Ongoing training for all staff
- Aerosol generated exposures are a potential risk within the dental surgery
- Standard IPC protocols apply
- AGEs need to be considered as high risk / low risk
- Standard PPE for low risk procedures considered as BASIC
- High risk procedures require FFP2, visor and gown as BASIC
- Use of rubber dam and high- volume suction are important mitigating measures
- Fallow period of 60mins required for high risk AGEs
- Oral mouth rinses not indicated
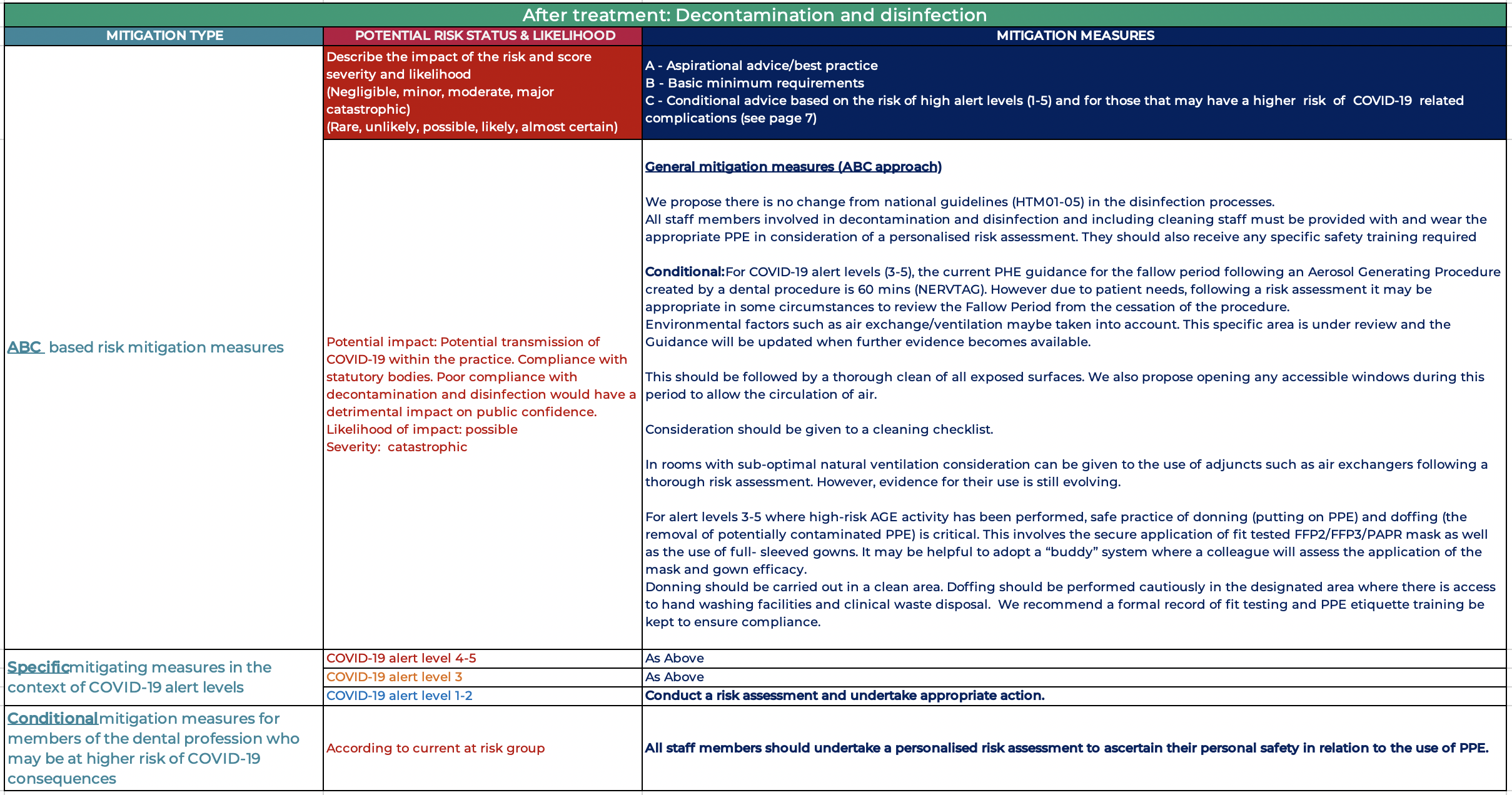
- Standard decontamination procedures should be followed
- Routine cleaning for low risk AGEs
- High risk AGEs require appropriate doffing of gown, with mask retained and removed outside the surgery
- A fallow time of 60 minutes is currently recommended, timed from cessation of the dental AGE
- Mitigating measures may be implanted
- to reduce this figure
- Floor cleaning should be undertaken at the end of each high-risk AGE or the end of each session.
- No paper records should be retained in the surgery during high risk AGEs or during the fallow period
- Scrubs should be changed daily and washed at the highest possible temperature
- Protocols reviewed regularly and reflect the level of risk
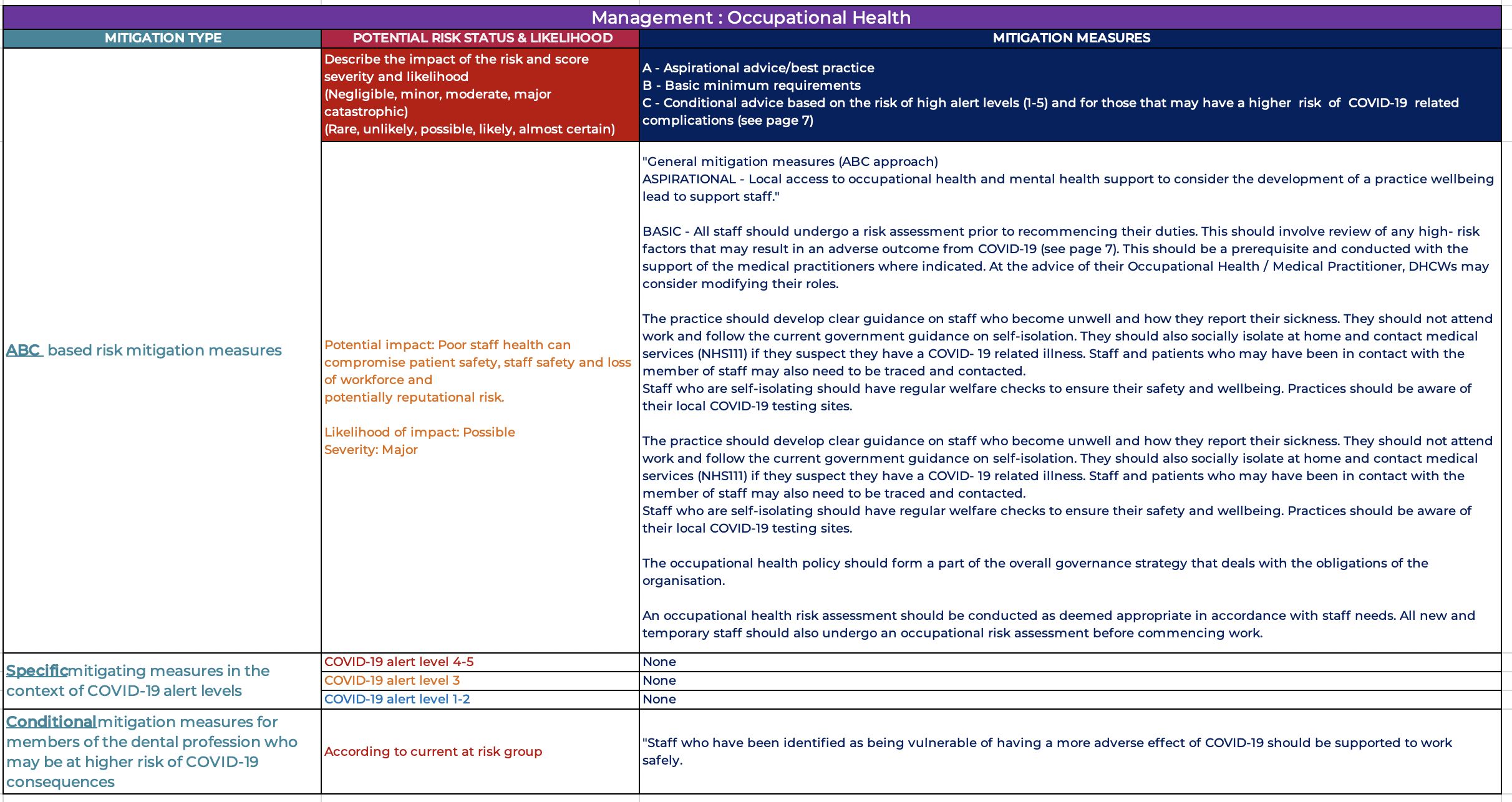
- Identify members of staff to fulfil specific duties:
Management lead/ Governance lead
Health and wellbeing lead
- Facilities prepared to support social distancing with appropriate signage / demarcation
- Risk assessment of staff prior to recommencement of work
- Access and occupational health support available for staff
- Appropriate training in place, including medical emergencies
- Stock control reviewed and ensure appropriate PPE available
How to read the tables / risk matrices
Domain: refers to the aspects of the patient journey in question (or the management section) and the sub-topics within it which the guidance covers. This is also repeated at the start of each technical section.
Risk Status: this part of the table describes the risk in question and makes a judgment about how likely the issue is to occur and what the effect of that would be without taking the specific measures or mitigating actions listed. The likelihood is measured as one of rare, unlikely, possible, likely or almost certain. The severity of the impact is measured as one of negligible, minor, moderate, major or catastrophic.
The mitigating actions we set out are judged to be proportionate to the risk status i.e. the most robust and stringent measures will be in place for risks with a rating of almost certain / catastrophic and the least stringent measures (or none at all) for rare/ negligible rated risks.
ABC based risk mitigation measures: the steps which should be taken to ensure safe practice. “General mitigations” are described in relatively limited detail and intended to apply across a domain, and are to be read as basic requirements (so “B” category).
“A” measures are aspirational and represent the best possible practice.
“B” (basic) measures represent a minimum standard which must be in place for the procedures or topic in question and reflect a balance of the safety requirements relative to the risk and alert level and practical operating and resourcing constraints.
“C” measures are conditional i.e. they denote basic measures (minimum requirements) in specific circumstances e.g. if a dentist or a patient are in a high-risk category for adverse outcomes form COVID 19 infection. “Specific mitigations” indicates where a measure we recommend is differentiated according to the COVID 19 alert level in place.
COVID-19 alert level refers to the UK government 5-level alert description (see our FAQ for fuller framework), where 5 is critical, 4 is severe, 3 is substantial, 2 is moderate and 1 is low. Because the impact on safe practice is very similar, we have generally grouped levels 5 and 4 together, and often 3, 4 and 5. Once the alert level has returned to 1, general dental practice minimum standards may well be those which existed before COVID-19 arrived in the UK.
- Post treatment the instrument box should be covered and left in the surgery
- Clinicians should go to doffing station & follow doffing guidelines, they must leave the clinical room with their eye protection and respirators still on.
- After a full hour has been given a terminal clean of full surgery doors, door handles any surfaces that are at risk of contact including floor using appropriate cleaning agent effective against enveloped viruses such as 1000ppm chlorine mix OR alternative disinfection effective against enveloped virus by "dirty nurse" with a FFP3 respirator on
- Post treatment disinfection should follow HTM: 01-05
Suggested Protocol if a Patient becomes unwell during an appointment in a UDC
If COVID-19 is considered possible when an appointment is already in progress, assess a suitable and safe point to bring any treatment to a close.
1. Isolate patient in surgery you are treating away from other patients. Provide mask and gloves for the patient and chaperone to put on. Provide water and tissues. Advise others not to enter the area. Put out isolation notices to prevent entry
2. If the patient is critically ill or requires emergency medical care, an ambulance should be requested, and the 999-call handler informed of COVID-19 risk. Normal medical emergency training is appropriate especially oxygen and asthma care if appropriate. Support breathing as primary concern.
3. Otherwise withdraw from the area, wash hands thoroughly with soap and water. Change PPE and discard in clinical waste. Don new PPE and apron.
4. If they are so unwell they cannot leave ask them where they have been in the building and clean all touched surfaces, open all doors, and windows. Turn up heating. Recruit help for other duties, such as reception.
5. Send all other patients home after updating their contact numbers/details. Once patients gone, shut practice. Put up PRACTICE CLOSED sign on front door.
6. Advise patient to contact NHS111 from their mobile in designated isolation area: –patient will need to state where they are calling from and provide contact details for the practice. If no patient mobile, staff to call on practice phone and relay responses to NHS111.
7. While waiting for advice from NHS111, communicate with the patient from outside area to check status. If you need to enter the area, wear personal protective equipment (PPE) in line with standard infection control precautions, gloves, disposable apron and surgical mask and keep exposure to a minimum. All PPE should be disposed of as clinical waste.
8. If a healthcare professional is required to enter the area to offer assistance, they should wear disposable gloves, disposable aprons and fluid-resistant surgical facemasks.
9. When patient has left the building, clean surgeries thoroughly and ALL communal areas down to front door and time allowed for aerosols to settle.